Researchers from the BU CTE Center have found that immune-related proteins could help differentiate between neurodegenerative diseases and provide additional candidates for biomarkers or new therapeutic targets.
One of the largest challenges in neuroscience is identifying and treating neurodegenerative diseases during life, as many are only able to be diagnosed after death.
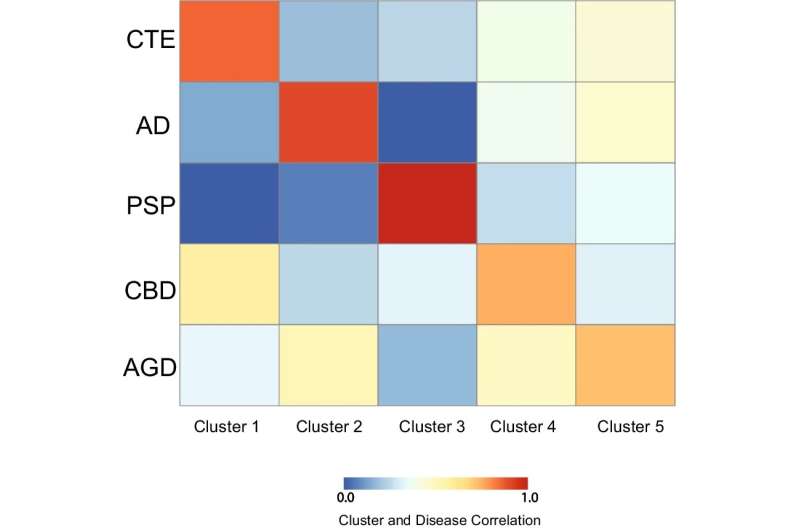
Additionally, several diseases can sometimes have overlapping clinical symptoms that makes diagnosis even more challenging, including Alzheimer's disease (AD), Chronic Traumatic Encephalopathy (CTE), progressive supranuclear palsy (PSP), corticobasal degeneration (CBD) and argyrophilic grain disease (AGD), which highlights the critical need for better ways to identify and distinguish during life.
"We identified the protein CCL21 was specific of CTE, FLT3L was selective of AD, and IL-13 was highest in PSP. This is novel since it provides more possible biomarkers to help better identify diseases like CTE, AD, PSP, CBD or AGD during life. Additionally, it helps us better understand the mechanisms behind each disease," says corresponding author Jonathan Cherry, Ph.D., a research health scientist at the VA Boston Healthcare System and assistant professor of pathology and laboratory medicine at Boston University Chobanian & Avedisian School of Medicine.





